According to the CDC, regular blood sugar monitoring is the best tool to prevent complications from diabetes and know if your diabetes plan is working. When checking is performed regularly, it helps you assess how well you are balancing your medication regimen, meal planning, and exercise to manage your diabetes
By monitoring your blood sugar, you can find out if your blood glucose levels are within your target range. This information is vital for not only you, but your Care Team as well. By tracking your glucose in a log form, you will see what affects your glucose on a day to day bases. Different variables will affect your glucose such as the type and amount of foods you eat, medications, and exercise. With this information, your diabetes Care Team, such as your Endocrinologist, Primary Care Doctor, and Certified Diabetes Educator or Dietitian, will be able to work with you to make the best decisions about your diabetes care plan.
Monitoring and keeping your glucose within target ranges will help prevent complications from diabetes, such as kidney disease, heart attack, amputations, blindness, or a stroke. Most people hesitate to check their glucose because they often feel ashamed by their numbers, but there is nothing to be ashamed of.
Your “numbers” is just data that reflects your total diabetes care including all medications. Remind yourself, if you find yourself discouraged, that tracking your glucose level is simply a way to know how well your treatment plan is working and whether that plan needs to change.
It can be confusing sometimes about when to check your glucose, what numbers to look for, etc. That’s why it’s strongly advised to establish these target goals and a monitoring schedule with your Care Team as it is personalized to each person. Below is a checklist that can help improve your diabetes care and consider bringing this to your next doctor's visit:
Doctor Visit Check List:
How do I check my glucose with my Blood Sugar Meter?
How often should I check my blood sugar?
What times should I check my blood sugar?
Should I bring my glucometer / glucose log to every follow up visit?
Are there patterns that show I need to make changes to my diabetes treatment?
What is my target blood sugar level?
Target Glucose Ranges
Target glucose ranges are personalized for each patient and should be discussed with your diabetes Care Team.
Standard guidelines from The American Diabetes Association suggests the following targets for most nonpregnant adults with diabetes:
Before a meal (fasting or pre-prandial plasma glucose): 80–130 mg/dL
1-2 hours after beginning of the meal (postprandial plasma glucose): Less than 180 mg/dL
How often should I check?
When beginning to monitor your blood glucose, it is important to have your Care Team determine how often you should check your glucose. Depending on the treatment plan, your frequency to check will vary. After that is established, you should create a monitoring schedule for yourself. It is also important to note that it is not advised, unless otherwise stated by your doctor, to check randomly. Checking randomly and too often can lead to diabetes burnout, which is when a person is overwhelmed with their management. Checking your fasting (pre-prandial) or after meal (post-prandial) glucose levels are commonly the most important for individuals with diabetes. Those who are taking insulin, pregnant, having a hard time controlling blood glucose levels, having low blood glucose levels without the usual warning signs or have ketones from high blood glucose levels are especially advised to monitor their glucose closely.
What should I be recording?
When you finish checking your glucose make sure you jot down the following:
Date/ day of the week
Time of the day
Glucose reading
If it was a fasting or a post-meal glucose check
If the reading surprises you, write a note to what may have contributed (ie. exercise, extra medications, skipping medications, skipping meals or overconsumption of food)
Compare these numbers to your target goals. Look at the trend at the end of the week. If your numbers are above your goal, contact your Care Team to discuss potential reasons why. If it is attributed to your diet, ask for a referral to see a dietitian who specializes in diabetes to help teach you ways to manage your blood sugar via diet therapy. If your levels are persistently below target, notify your doctor and inform them about these hypoglycemic episodes. It may be time to change your diabetes care plan.
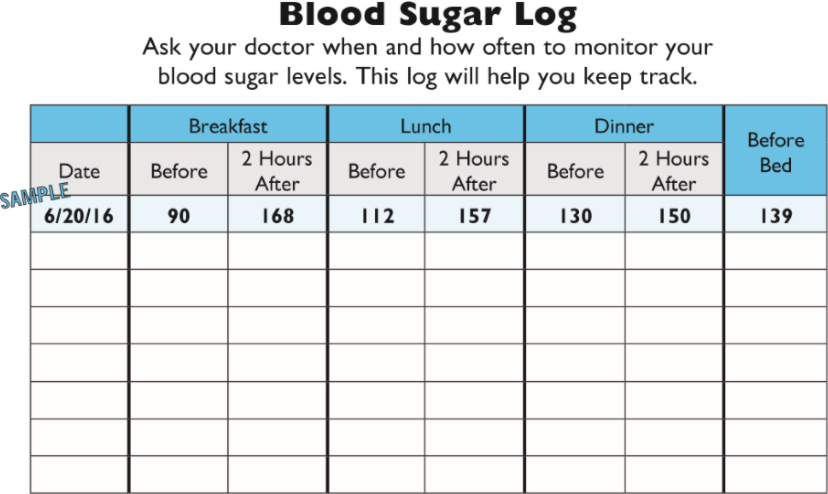
Here are some sample glucose logs from the NYC Department of Health: